
Research suggests that COVID-19 hospitalizations could have been prevented without four common pre-existing conditions. Credit: Gerald J. and Dorothy R. Friedman School of Nutrition Science and Policy at Tufts University
Model suggests higher risk based on race and age, provides insights to reduce impact on disease.
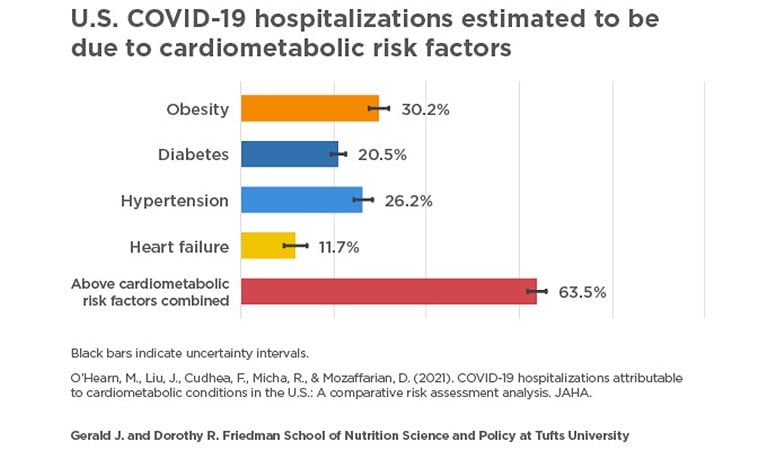
A model study suggests a majority of adults COVID-19 hospitalizations across the country are attributable to at least one of four pre-existing conditions: obesity, hypertension, diabetes, and heart failure, in that order.
The study, published today (Feb. 25, 2021) in the Journal of the American Heart Association JAHA) and led by researchers from the Gerald J. and Dorothy R. Friedman School of Nutrition Science and Policy at Tufts University, used a mathematical simulation to estimate the number and proportion of national COVID-19 hospitalizations that could have occurred If the Americans had not, are suffering from four major cardiometabolic disorders. Each condition has been strongly associated with an increased risk of poor outcomes with COVID-19 infection in other studies.
“While newly approved COVID-19 vaccines will eventually reduce infections, we still have a long way to go to get to that point. Our findings call for interventions to determine whether improving cardiometabolic health will reduce hospitalization, morbidity and healthcare stress from COVID-19, ”said Dariush Mozaffarian, lead author and Dean of the Friedman School. “We know that changes in nutritional quality alone, even without weight loss, rapidly improve metabolic health within just six to eight weeks. It is crucial to test such lifestyle approaches to reduce severe COVID-19 infections, both for this pandemic and for future pandemics likely to come. “
The researchers estimate that among the 906,849 total COVID-19 hospitalizations that had occurred in U.S. adults on November 18, 2020:
- 30% (274,322) was due to obesity;
- 26% (237,738) was due to hypertension;
- 21% (185,678) was due to diabetes; and
- 12% (106,139) was due to heart failure.
In epidemiological terms, the attributable share represents the percentage of COVID-19 hospitalizations that could have been prevented without the four conditions. In other words, the study found that the individuals may still be infected, but may not be severe enough to require hospitalization. When the numbers for the four conditions were combined, the model suggests that 64% (575,419) of COVID-19 hospitalizations could have been prevented. A 10% reduction in the national prevalence of each condition, if combined, could prevent about 11% of all COVID-19 hospitalizations, according to the model.
The four conditions were chosen based on other published research from around the world, showing that each is an independent predictor of serious outcomes, including hospitalization, in people infected with COVID-19. The specific risk estimates for each condition came from a published multivariable model involving more than 5,000 COVID-19 patients previously diagnosed in the New York City pandemic. The researchers used other national data to model the number of COVID-19 hospital admissions nationwide; the breakdown of these hospital admissions by age, gender and race; and the estimated distribution of the underlying co-morbidities among adults infected with COVID-19. They then estimated the ratios and numbers of COVID-19 cases that became severe enough to require hospitalization due to the presence of one or more of the conditions.
“Healthcare providers should educate patients at risk for severe COVID-19 and consider promoting preventive lifestyle measures, such as improved nutritional quality and physical activity, to improve overall cardiometabolic health. It is also important for health care providers to be aware of the health inequalities that people with these conditions often face, ”said lead author Meghan O’Hearn, a PhD student at Friedman School.
The model estimated that age and race / ethnicity led to differences in COVID-19 hospital admissions due to the four conditions. For example, it was estimated that about 8% of COVID-19 hospitalizations among adults under 50 years of age were due to diabetes, compared to about 29% of COVID-19 hospitalizations among those aged 65 and older. In contrast, obesity equally adversely affected COVID-19 hospital admissions in all age groups.
At any age, COVID-19 hospitalizations attributable to all four conditions were higher in black adults than in white adults and generally higher in diabetes and obesity in Hispanic adults than in white adults. For example, diabetes among adults aged 65 and older is estimated to cause about 25% of COVID-19 hospital admissions in white adults, versus about 32% in black adults and about 34% in Hispanic adults.
When the four conditions were considered combined, the proportion of attributable hospitalizations was highest in black adults of all ages, followed by Hispanics. For example, in young adults aged 18-49, the four conditions combined accounted for about 39% of COVID-19 hospital admissions among white adults, versus 50% among black adults.
National data shows that Black and Hispanic Americans are the worst affected by COVID-19. Our findings support the need to prioritize the distribution of vaccines, good nutrition and other preventive measures for people with cardiometabolic disease, especially among groups most affected by health inequalities, ”said Mozaffarian. “Policies aimed at reducing the prevalence of these four cardiometabolic disorders among black and Hispanic Americans should be part of any state or national policy discussion aimed at reducing health inequalities from COVID-19.”
data
The model used existing data from various sources. Hospital admissions by age, gender, race, and ethnicity came from the CDC’s COVID-NET system, which tracks COVID-19 hospital admissions in 14 participating states. National COVID-19 hospital admissions data came from The COVID Tracking Project, a volunteer organization that collects data from all 50 states on the COVID-19 outbreak in the U.S. These two datasets were combined to provide COVID-19 hospital admissions nationally. to be estimated per population subgroups. The data on the nationwide distribution of the four conditions comes from the most recent National Health and Nutrition Examination Survey (NHANES), a nationally representative study in which participants undergo medical examinations and laboratory tests. Data on the association between COVID-19 hospital admissions and each of the four conditions came from a study of factors associated with hospitalization in people with COVID-19 in New York City.
Limitations
The authors note that association does not equate to causality, and the modeling approach does not prove that reductions in the four conditions will reduce COVID-19 hospital admissions. Assumptions were based on the limited data available on the distribution of the cardiometabolic disease among COVID-19-infected US adults, the demographic breakdown of COVID-19 hospital admissions nationally, and the strongest evidence to date on links between cardiometabolic disease and poor disease. COVID-19 results.
Authors
Other authors of the study include Frederick Cudhea and Renata Micha of the Friedman School, and Junxiu Liu, a postdoctoral fellow at Friedman School at the time of the study, now assistant professor at the Icahn School of Medicine on Mount Sinai.
Financing
This work was supported by two awards from the National Institute of Health’s National Heart, Lung, and Blood Institute (R01HL130735 and R01HL115189). The content is the sole responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. See the study for conflicts of interest.
Quote
O’Hearn, M., Liu, J., Cudhea, F., Micha, R., & Mozaffarian, D. (2021). COVID-19 Hospitalizations Attributable to Cardiometabolic Disorders in the US: A Comparative Risk Analysis. Journal of the American Heart Association