
ICU beds across Southern California are falling to critical levels, with capacity dropping to 1% in Ventura County and 0% in Riverside County, while Los Angeles County – home to 10 million people – has fewer than 100 beds available had.
But the worst of the wave is yet to come, experts say. In LA County, more than 4,400 people have been hospitalized with COVID-19, and officials said that number could rise to 5,000 by the weekend.
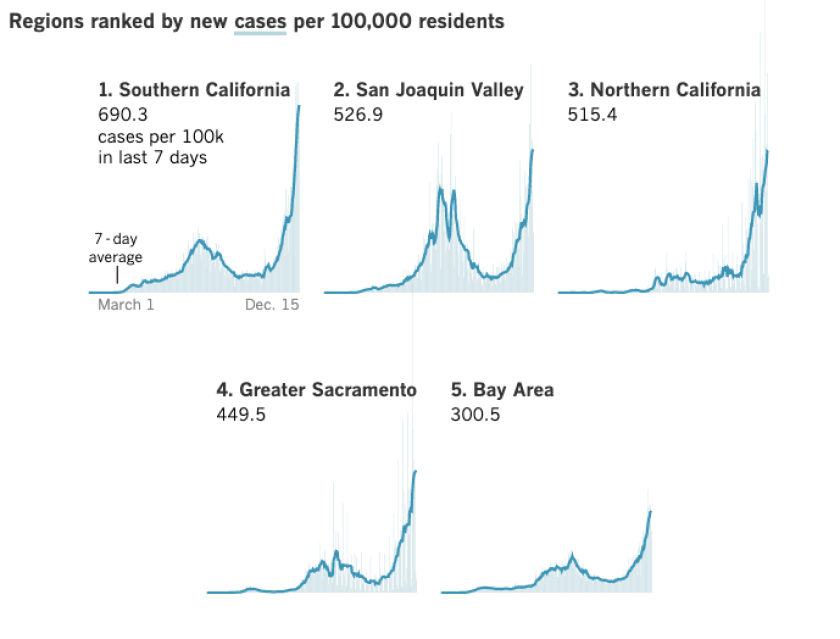
The shortages come as the coronavirus continues to rage in the state. A count by county from the Los Angeles Times showed an unprecedented 42,129 cases reported Monday. That number breaks the one-day record of December 8, when 35,400 cases of coronavirus were recorded.
“Our reality is terrifying right now,” said Barbara Ferrer, LA County’s director of health.
In LA County, hospital admissions in COVID-19 are now six times higher than in mid-October. On Sunday, there were 935 coronavirus patients in LA County’s limited supply of intensive care beds – more than a four-fold increase from Nov. 1.
In Ventura County, health officer Dr. Robert Levin are dismayed at people who persist in celebrations, indoor church services and youth sporting events who are currently banned due to the extraordinary public health crisis.
The numbers are getting astronomical. There will be people who don’t have to die, ”Levin said Monday.
Across Southern California, available ICU capacity fell to 2.7% Monday from 4.2% a day earlier. In the San Joaquin Valley, it has dropped to 0% again, meaning some critically ill patients have to be housed in areas of hospitals not normally designed to care for ICU patients, which can increase mortality.

“A lot of people may think this is just not something to be really worried about because hospitals can just add more beds. The reality is that every bed needs to be staffed by trained and skilled health workers, and we don’t have an endless supply of health workers, and those who save lives here every day are exhausted, ”Ferrer said.
“And they are discouraged by the reality that this isn’t the way it should be,” she added. “The best thing anyone can do now is stay at home as much as possible and only go out for work, school, exercise or essential services.”
LA County is so slammed by COVID-19 patients that during certain periods on Sunday, 81% of hospitals receiving patients who came from 911 calls were forced to temporarily divert some ambulance patients elsewhere, said Dr. Christina Ghaly. , the director of LA County. of health services.
Ghaly said officials are bracing to aggravate hospital admissions because people infected with Thanksgiving become so sick they must be admitted. There are about 500 new daily COVID-19 hospital admissions in LA County, and that number could exceed 700 in a week, Ghaly said.
“We have to brace ourselves for this [hospital] case volume has not yet peaked and will continue to grow, ”said Ghaly.
Wait five hours to send ambulance patients to hospitals
LA County is also experiencing the kind of lengthy delays in transferring patients from ambulances to hospitals that Orange County reported last week.
“We are aware that in certain hospitals across the country there are prolonged defecation times for ambulance patients that often exceed four hours, five hours,” Ghaly said.
On Monday, LA County averaged nearly 10,700 new coronavirus cases per day and 58 new COVID-19 deaths per day for the past week – both at and near the records.
Ferrer said she hoped the stay-at-home order around Christmas would stabilize or reduce the number of new daily coronavirus cases.
Whether that happens will depend on whether Angelenos “actually adheres to this new ‘Safer Home’ order,” Ferrer said.
Younger adults are the most likely to spread the virus, Ferrer said, but it’s the oldest adults who die the highest when infected.
“And this is a tragedy that can be prevented, because those most vulnerable to serious illnesses from COVID-19 can be protected by everyone,” Ferrer said. and avoid us with non-household members. “
Health officials are concerned about opposing health regulations
There are concerns about failure to follow orders. After LA County issued a ban on alfresco dining in restaurants, the city of Manhattan Beach implemented a plan to allow residents to continue to use newly built outdoor dining areas as public seating for people to sit and dine. Dr. LA County health officer Muntu Davis has asked the city to “refrain from bypassing a workaround for the temporary suspension of outdoor dining.”
“By placing tables and chairs next to restaurants, the city of Manhattan Beach violates and defeats the purpose of the county order and is far from protecting public health,” Davis wrote. The seats in the newly designated outdoor seating match the restaurants’ stock tables and chairs and are not owned by the city, Davis wrote.
The number of coronavirus cases in Manhattan Beach has tripled since mid-September, Davis wrote.

A couple enjoys a meal on Manhattan Beach Boulevard in Manhattan Beach on December 4.
(Wally Skalij / Los Angeles Times)
In Ventura County, health officer Levin raised the alarm when COVID-19 hospital admissions there shattered records and broke the record for 10 consecutive days. On Sunday, 181 coronavirus-infected people were in the county’s hospitals, up 72% from the peak of the increase in July.
Two weekends ago, about 80 soccer players gathered in a park in Simi Valley; sports tournaments take place in other counties with volleyball and baseball players, and in those situations, people didn’t wear masks, Levin said. Some church services are still held indoors, with audience sometimes sitting shoulder to shoulder, in violation of the rules requiring church services to be held online or out of the home.
‘These are not just old people who are sick and die’
At the Oaks mall in Thousand Oaks, there was a report of hundreds of people gathering to sing Christmas carols, many without masks, Levin said. And he’s heard of parties of up to 200 people and residents attending drive-in concerts but getting out of their cars anyway.
Singing is an extremely high-risk activity and has been documented to spread the coronavirus. In one choir practice, dozens of people infected with the corona virus and two people died in Washington State.
“What’s understandable about this?” Levin said at a press conference. “None of these justifications are acceptable in the face of the pandemic. We should all work together, just as we would any war.
‘It is incomprehensible to me. It’s astonishing. It’s also irresponsible, ”said Levin. “COVID is so widespread in our province that 1 in 10 COVID tests we perform are positive.
“It’s too easy to run into someone with COVID these days and not know you’re being exposed,” he said. There are now 49 outbreaks in long-term care facilities in Ventura County.
Levin said one of his daughters works at a hospital in Sacramento. ‘She said to me,’ Daddy, I’m looking around the hospital: these aren’t just old people who are sick and dying. These are young people, like me. ‘It’s heartbreaking. And she is right. “
‘We had to tell family … that their loved ones are not coming home’
One of the long-term consequences for some younger people who are infected is the so-called ‘long-hauler’ syndrome, where survivors can suffer from persistent shortness of breath and a ‘foggy head’ – a constant state of confusion and clouded thinking that can last for months. Levin said.
Some of these people were joggers. We don’t know if that will be permanent or not, ”said Levin. “If we all worked together, came together – and I mean figuratively, so spiritually – for just three or four weeks, our infections would go away. They would plummet. And our companies could open. ”
Dr. Mark Lepore, an intensive care physician at Ventura County Medical Center, said he expects Ventura County to exceed hospital capacity, “and what the capacity looks like is coming to the hospital and not having a room to enter or an employee to take care of you. ”
“The hardest thing about caring for COVID… is the lack of families who can see their loved ones, and it’s a terrible thing to see,” Lepore said. “It’s how slow and insidious the COVID is that it hits the body. You have symptoms for the first eight days, and then you just don’t recover. “
The fever may go away, but the shortness of breath can last to the end. “We’ve had to tell relatives that their loved ones aren’t coming home, and it’s awful,” said Lepore.
Lepore urged people not to get together for Christmas: “Just tell them you’ll see them next Christmas. This is so important: we don’t want your family members to get sick and receive care. “
The governor defends the order to stay at home
Gavin Newsom said Monday that there are some early signs that the new stay-at-home order – which was in effect for most of the state for a week – was starting to work to ease the movement of Californians.
“That saves time,” Newsom said.
The governor made the comment on the same day that health workers in Hollywood were among the first Californians to receive the COVID-19 vaccine. While the news has been greeted with optimism, the vaccine is coming too late to prevent infection in people exposed to the virus over Thanksgiving.
Amid complaints about the economic burden of the stay-at-home order, Newsom and other officials have championed it as a sensible way to protect lives and the economy once the vaccine is widely distributed.
“Once this pandemic is over, this condition will recover more resilient and vibrant than ever,” Newsom said Monday. “And so the most important thing we can do, from an economic perspective, is to pay attention to public health. Focus on reducing the spread of this virus. “
UCLA economists released an optimistic forecast last week, predicting that the US economy will see “a gloomy COVID winter and a buoyant vaccine spring” followed by solid growth for several years.
Newsom and health officials have defended California’s approach to the pandemic as one that saved lives. Of the 50 states, the District of Columbia and Puerto Rico, California has the 39th highest cumulative number of coronavirus cases per 100,000 residents and the 39th highest cumulative number of COVID-19 deaths per 100,000 residents.
Times contributors Sean Greene and Margot Roosevelt contributed to this report.