A recent study by US researchers shows how the 501Y.V2 variant of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), characterized by several mutations, can escape neutralization by the current first wave of anti-SARS-CoV – Re-infect 2 antibodies and possibly reparative COVID-19. The paper is currently available on the bioRxiv * preprint server.

As many variants of SARS-CoV-2 emerge and then crowd out the first wave viruses, it is crucial not only to assess their relative transmissibility and virulence in causing coronavirus disease (COVID-19), but also their tendency to escape antibody neutralization .
Of paramount importance are variants with mutations that can affect the interaction of the viral spike receptor binding domain (SRBD) with the viral receptor on host cells, the angiotensin converting enzyme 2 (ACE2), which is an entry point for the coronavirus.
Variants with greater binding affinity for ACE2 are more likely to spread. In addition, transmissibility has been linked to mortality, as an inevitable increase in the number of infections caused by the new variants will result in a higher rate of illness and death.
However, these dire consequences of more rapid and widespread infections may also be exacerbated by a loss of efficacy of currently available antibody-based treatments and vaccines and a decrease in protective immunity in individuals previously infected with a ‘first wave’ virus.
To improve our understanding of the risks of individual or combined mutations in these ‘second wave’ variants, a research group from the California company ImmunityBio conducted a computational analysis of the interactions of the S RBD with human ACE2.

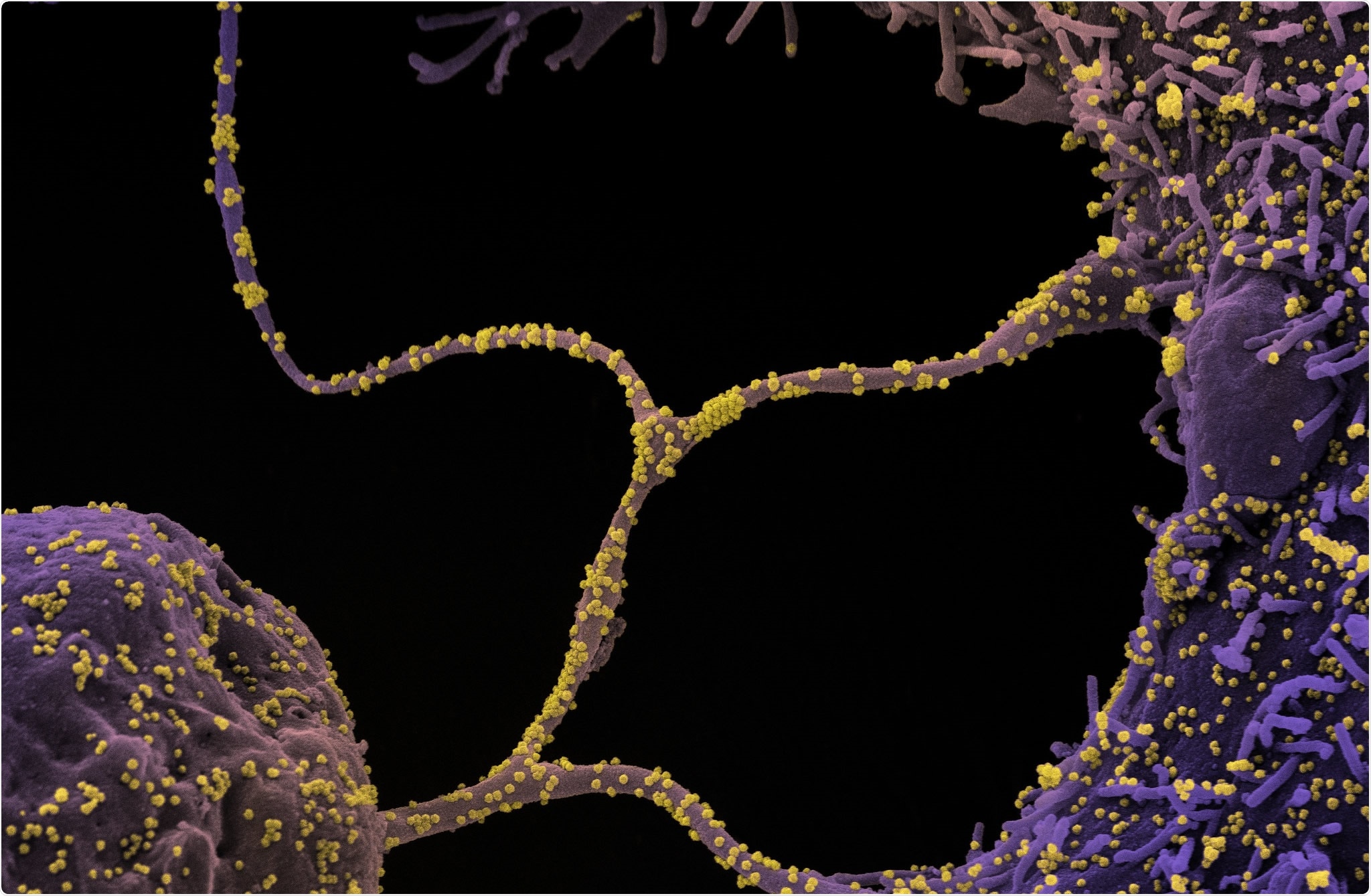
The K484 substitution in the new South African variant increases the affinity of the spike receptor binding domain (S RBD) for ACE2. (a, b) The positions of the E484K (red), K417N (cyan) and N501K (purple) substitutions on the interface of the 501Y.V2 variant S RBD – hACE2 interface are shown. hACE2 residues closest to the mutated RBD residues are shown as thin sticks. The E484K mutation is located in a highly flexible loop region of the interface, K417N in a region of lower probability of contact and N501K at a second high affinity point of contact. (c) The range of motion available for the loop containing residue 484 is shown by PCA from MD simulation of a first wave sequence11,13. (d) MD simulation performed in the presence of all 3 substitutions reveals that the loop region is closely linked (black arrow) to hACE2. A key contact pair is circled. (e) Compared to K484, when E484 (‘wild type’) is present with the Y501 variant only, the loop is not so closely connected (arrow).
In silico simulation methods
In this study, the researchers used millisecond-scale MD simulation methods to investigate mutations (E484K, K417N and N501Y) at the S RBD-ACE2 interface in the fast-spreading South African variant 501Y.V2 – and their effects on the RBD binding affinity. and peak glycoprotein conformation.
The wild-type ACE2 / RBD complex is made up of the cryoelectron microscopy structure. In addition, ten copies of each RBD mutant were minimized, equilibrated and simulated, and the processed minimization took place in two stages.
Finally, principal component analysis (PCA) was performed using the full set of simulations of the triple mutant, E484K and N501Y systems. Simulation structures were extrapolated to the eigenvectors for each mutation system.
The great escape from neutralization
The study revealed a greater affinity of K484 S RBD for ACE2 as compared to E484, as well as the greater chance of modified conformation compared to the original structure. In fact, this may represent mechanisms by which the new 501Y.V2 viral variant could replace the original SARS-CoV-2 strains.
More specifically, both E484K and N501Y mutations showed increased affinity of S RBD for human ACE2 receptor, while E484K was able to switch the charge on the flexible loop region of RBD, resulting in the formation of new beneficial contacts.
The aforementioned improved affinity is a likely culprit for a faster spread of this variant due to its greater transmissibility, which is a major reason why it is important to detect these mutations and act in a timely manner.
In addition, the induction of conformational changes is responsible for the escape of the 501Y.V2 variant (distinguished from the B.1.1.7 UK variant by the presence of the E484K mutation) from neutralization by existing anti-SARS-CoV-2 antibodies and re-infect recovering individuals with COVID-19.
Implications for further vaccine design
“We believe that the MD simulation approach used here is similarly a tool to be used in the arsenal against the ongoing pandemic, as it provides insight into the likelihood that mutations alone or in combination could have effects that affect the ongoing pandemic. efficacy of existing therapies or vaccines, ”say the authors of this study.
“We suggest that vaccines whose efficacy is largely dependent on humoral responses to the S antigen are inherently limited by the emergence of new strains and are dependent on frequent redesign,” they add.
On the other hand, a vaccine that elicits a powerful T cell response is much less subject to changes due to successive mutations and thus offers a better and more efficient approach to protection against this disease.
Finally, the ideal vaccine would also contain a second, conserved antigen (such as the SARS-CoV-2 nucleocapsid protein), which would likely elicit an effective humoral and cell-mediated immune response – even when faced with a rapidly evolving virus.
*Important announcement
bioRxiv publishes preliminary scientific reports that have not been peer reviewed and therefore should not be considered conclusive, serve clinical practice / health-related behavior, or be treated as established information.