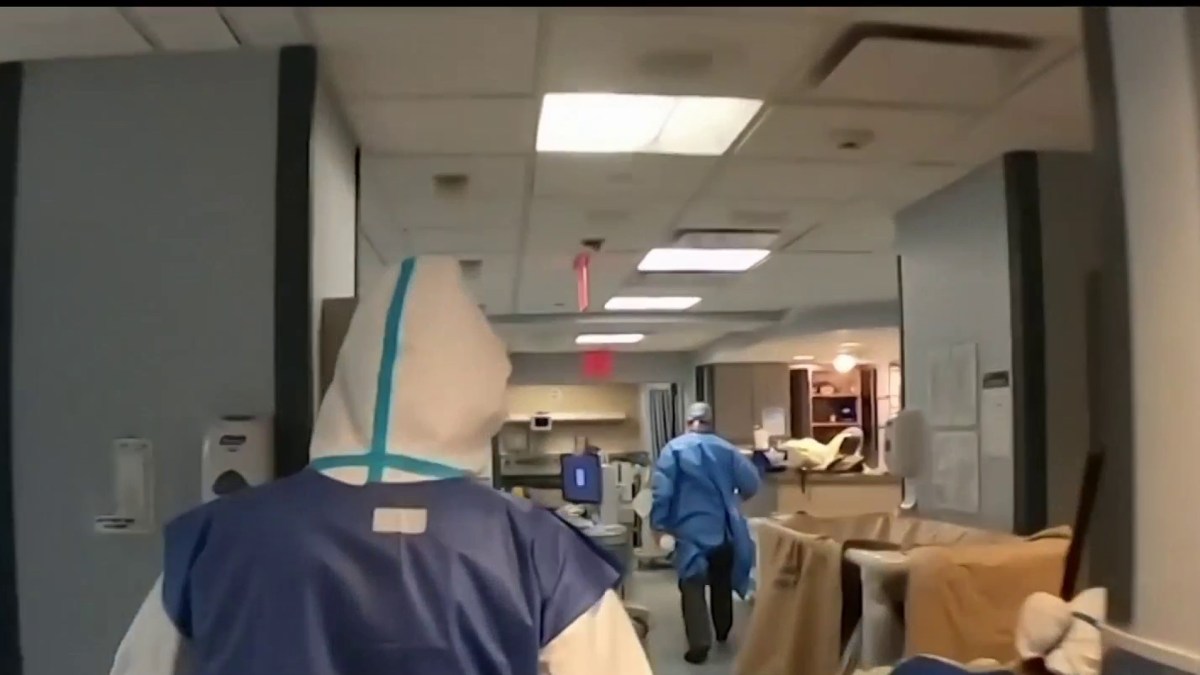
Hospitals in California are fighting to find beds to house patients amid fears that the explosive rate of coronavirus contamination will deplete resources and health workers.
On Saturday, nearly 17,400 people were hospitalized with confirmed or suspected COVID-19 infections – more than double the previous peak reached in July – and a state model using current data to predict future trends shows that the number could reach an unfathomable 75,000 by mid-day. -January.
More than 3,600 confirmed or suspected COVID-19 patients were in intensive care.
Some areas of California are “just about to be inundated,” said Dr. Anthony Fauci, the nation’s top infectious disease expert, at an event hosted by the California State University System.
Corona Regional Medical Center southeast of Los Angeles has converted an old emergency room to treat nearly double the usual number of ICU patients. It uses space in two disaster tents to triage ER patients, because the emergency room is filled with patients who need to be hospitalized.
Ambulances can sit for two hours unless they bring in patients with critical life or death emergencies.
“There is, in a manner of speaking, no room in the inn,” said director Mark Uffer of the hospital. “Literally every nook and cranny of the hospital is used.”
It’s a scene that takes place all over California. According to state data on Friday, all of Southern California and 12-county San Joaquin Valley in the north had exhausted their capacity for regular intensive care units and some hospitals have begun to use “surge” space.
In badly affected Fresno County in central California, a new 50-bed alternative care facility opened Friday near the community’s regional medical center. The beds for COVID-19 negative patients will free up space in regional hospitals, where only 13 of the roughly 150 ICU beds were available Friday, said Dan Lynch, the director of the emergency medical services department.
NBCLA’s Whitney Ashton talks to nurse Alice Benjamin about the questions surrounding the COVID-19 vaccines recently approved by the FDA for emergency authorization. As seen on NBCLA on Friday, December 18, 2020.
Lynch said he expects they will have to use the Fresno Convention Center, which can accommodate up to 250 patients, given current demand.
Fresno and three neighboring counties have also taken the unprecedented step of sending paramedics on emergency calls to evaluate people. They won’t be taken to the emergency room if they can go to an emergency room or wait a few days to talk to their doctors, Lynch said.
Some hospitals have canceled non-essential elective surgeries, such as hip replacements, which may require beds that may soon be needed for COVID-19 patients. Others extend staff hours or move patients to free up space.
‘I’m not going to soften this. We are being crushed, ”says Dr. Brad Spellberg, chief medical officer of the Los Angeles County-USC Medical Center, which has more than 600 beds and is one of the largest hospitals in the county.
Spellberg said every day at his hospital has started for the past week with no available intensive care beds and a struggle to find space in areas that don’t usually treat critical patients, such as post-surgery recovery areas.
“And it’s not just COVID patients,” he said. “They are car accidents and heart attacks and victims of violence. They need a place to get critical care.”
Ever-increasing demand can also put pressure on human resources.
“We still have physical beds available, but we need staff to care for patients. It doesn’t do much good to be in a bed without someone taking care of you, ”said Dr. Amy Herold, chief medical officer at Queen of the Valley Medical Center in Napa, on the San Francisco Chronicle. “People are working overtime over and over and they’re exhausted and it’s only getting worse.”
We revisit some of the people who have helped health workers since the start of the pandemic. Hetty Chang reports for NBC4 News on December 18, 2020 at 11 p.m.
John Chapman, president and chief executive of San Antonio Regional Hospital in Upland, said telemetry nurses monitoring patients’ vital signs should not oversee more than four people, but could hire five or six because of the number of cases.
“It certainly increases the risk of something going wrong,” he said.
Many emergency rooms are already using outdoor tents to make more room, said Dr. Marc Futernick, a Los Angeles emergency room physician who sits on the board of the California division of the American College of Emergency Physicians. A hospital that has made the most of its outdoor overflow tent is expanding to a nearby gym, he said.
Still, coronavirus cases haven’t peaked in this third and most devastating wave, and that means more drastic measures are on the horizon.
Many hospitals are preparing for the possibility of rationing care. Recently, a document circulated among doctors in the four Los Angeles County hospitals asking them to change strategies: Instead of trying everything to save a life, their goal during the crisis is to save as many patients as possible.
“A compromise in the standard of care is inevitable; it is not that an entity, system or country chooses to limit resources, it is that the resources are clearly not available to provide care in a regular manner,” the document said obtained by the Los Angeles Times.
The director of the county’s Health Services, Dr. Christina Ghaly, said the guidelines were not in effect as of Friday night, but they were essential to develop as the wave has arrived and “the worst is yet to come.”
As of Saturday, the country’s most populous state recorded more than 43,000 new confirmed cases and 272 deaths, both among the highest one-day totals during the pandemic. In the past week, California has reported more than a quarter of a million cases and 1,500 deaths.
California has begun to receive new COVID-19 vaccines. But available doses are too scarce and too late to have an immediate impact on the rising infection rate.
The latest explosion of cases has been linked to ignoring social aloofness rules over the Thanksgiving holiday. Healthcare officials and workers expressed frustration that many people are not adhering to state-imposed safety rules designed to slow that pace.
“Whatever comes, I don’t think any of us will make it,” Uffer said. “You have a dam about to break, and you have to stop pouring water into the dam.”
If people don’t curtail upcoming vacation trips and gatherings, the state could see a “wave on a wave,” Fauci said.
“I’m afraid it will be worse than what we’ve seen in New York,” Futernick said. “When hospitals in New York became overwhelmed, healthcare providers poured in from all over the country.”
“None of that is happening now, and it cannot happen because it is busy everywhere,” said Futernick. “No cavalry is coming.”
Saturday night, Apple Inc. announced that it is temporarily closing all 53 stores in California due to the coronavirus outbreak. The move came after new state mandates cut the number of stores to 20 percent.
“Due to the current Covid-19 conditions in some of the communities we serve, we are temporarily closing stores in these areas,” Apple said in a statement obtained by the Bloomberg news service. “We are taking this step with great caution as we are monitoring the situation closely and we look forward to having our teams and customers back as soon as possible.”
____
Taxin reported from Orange County. Associated Press writers Adam Beam and Don Thompson contributed from Sacramento and Janie Har from San Francisco.