News release
Wednesday December 30, 2020
Results from a study of 19 deceased patients suggest that brain damage is a byproduct of a patient’s disease.
In an in-depth study of how COVID-19 affects a patient’s brain, researchers at the National Institutes of Health consistently found features of damage caused by thinning and leaky brain blood vessels in tissue samples from patients who died shortly after contracting the disease. In addition, they saw no signs of SARS-CoV-2 in the tissue samples, suggesting that the damage was not caused by a direct viral attack on the brain. The results were published as correspondence in the New England Journal of Medicine.
“We found that the brains of patients infected with SARS-CoV-2 can be susceptible to damage to microvascular blood vessels. Our results suggest that this may be due to the body’s inflammatory response to the virus, ”said Avindra Nath, MD, clinical director of NIH’s National Institute of Neurological Disorders and Stroke (NINDS) and the study’s senior author. “We hope these results will help physicians understand the full spectrum of patients’ problems so that we can come up with better treatments.”
Although COVID-19 is primarily a respiratory disease, patients often experience neurological problems, including headache, delirium, cognitive impairment, dizziness, fatigue, and loss of sense of smell. The disease can also cause patients to develop strokes and other neuropathologies.
Several studies have shown that the disease can cause inflammation and damage to blood vessels. In one of these studies, the researchers found evidence of small amounts of SARS-CoV-2 in the brains of some patients. Yet scientists are still trying to understand how the disease affects the brain.
In this study, the researchers conducted an in-depth examination of brain tissue samples from 19 patients who died after experiencing COVID-19 between March and July 2020. Samples from 16 of the patients were provided by the Office of the Chief Medical Examiner in New York City, while the other 3 cases were provided by the Department of Pathology at the University of Iowa College of Medicine, Iowa City. The patients died at different ages, from 5 to 73 years old. They died within a few hours to two months of reporting symptoms. Many patients had one or more risk factors, including diabetes, obesity and cardiovascular disease. Eight of the patients were found dead at home or in public settings. Another three patients collapsed and died suddenly.
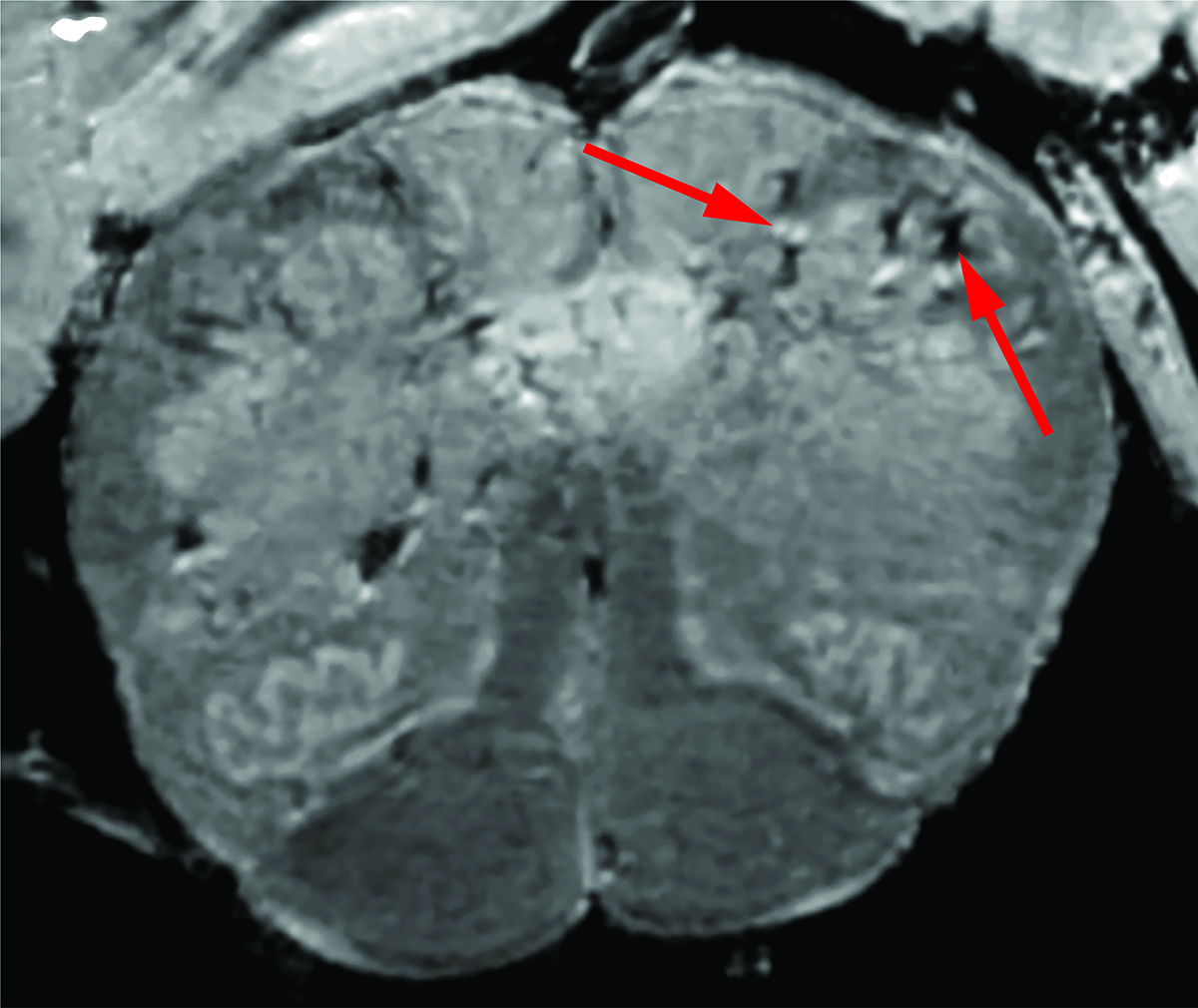
Initially, the researchers used a special, powerful Magnetic Resonance Imaging (MRI) scanner, which is 4 to 10 times more sensitive than most MRI scanners, to examine samples of each patient’s olfactory bulbs and brain stems. These regions are believed to be highly susceptible to COVID-19. Olfactory bulbs regulate our sense of smell, while the brainstem regulates our breathing and heart rate. The scans showed that both regions had an abundance of bright spots called hyperintensities, which often indicate inflammation, and dark spots called hyposensitivities, which represent bleeding.
The researchers then used the scans as a guide to take a closer look at the spots under the microscope. They found that the bright spots contained blood vessels that were thinner than normal, and sometimes blood proteins, such as fibrinogen, leaked into the brain. This turned out to trigger an immune response. The spots were surrounded by T cells from the blood and the brain’s own immune cells called microglia. In contrast, the dark spots contain both clotted and leaky blood vessels, but no immune response.
“We were totally surprised. We originally expected to see damage caused by a lack of oxygen. Instead, we saw multifocal damage areas commonly associated with strokes and neuro-inflammatory conditions, ”said Dr. Nath.
Finally, the researchers saw no signs of infection in the brain tissue samples, although they used different methods to detect genetic material or proteins from SARS-CoV-2.
“So far, our results suggest that the damage we have seen may not have been caused by the SARS-CoV-2 virus that directly infects the brain,” said Dr. Nath. “We plan to investigate in the future how COVID-19 damages the blood vessels of the brain and whether it causes some of the short and long term symptoms that we see in patients.”
This study was supported by the NIH Intramural Research Program at the National Institute of Neurological Disorders and Stroke (NS003130) and an NIH grant (NS109284).
NINDS (https://www.ninds.nih.gov) is the leading funder of brain and nervous system research. NINDS ‘mission is to seek fundamental knowledge about the brain and nervous system and use that knowledge to reduce the burden of neurological disorders.
About the National Institute on Aging (NIA): NIA leads the US federal government’s efforts to conduct and support research on aging and the health and well-being of the elderly. Learn more about age-related cognitive change and neurodegenerative diseases through the NIA’s Alzheimer’s and Related Dementias Education and Referral (ADEAR) Center website. For information on a wide variety of aging topics, visit the NIA main website and stay tuned.
About the National Institutes of Health (NIH):
NIH, the national medical research agency, includes 27 institutes and centers and is part of the United States Department of Health and Human Services. NIH is the premier federal agency that conducts and supports basic, clinical, and translational medical research, investigating the causes, treatments, and cures for both common and rare diseases. For more information about NIH and its programs, visit www.nih.gov.
NIH … Turning Discovery into Health®
Article
Lee MH, Perl DP, Nair G, Li W, Maric D, Murray H, Dodd SJ, Koretsky AP, Watts JA, Cheung V, Masliah E, Horkayne-Szakaly I, Jones R, Stram MN, Moncur J, Hefti M, Folkerth RD, Nath A. Microvascular injury in the brains of patients with COVID-19. New England Journal of Medicine, December 30, 2020 DOI: 10.1056 / NEJMc2033369.