SALT LAKE CITY – The number of patients at Primary Children’s Hospital diagnosed with a coronavirus-related complication has doubled from the past two months.
In fact, there are now more than 1,500 confirmed cases of multisystem inflammatory syndrome in children, also known as MIS-C. The syndrome develops after the child is infected with SARS-CoV-2.
As medical experts try to unravel the long-term effects of COVID-19, officials at Primary Children’s Hospital announced Tuesday that they will begin the first study of MIS-C.
The long-term outcomes after the multisystem inflammatory syndrome in children called the MUSIC study will try to answer how MIS-C affects children who were diagnosed with it five years after they developed it.
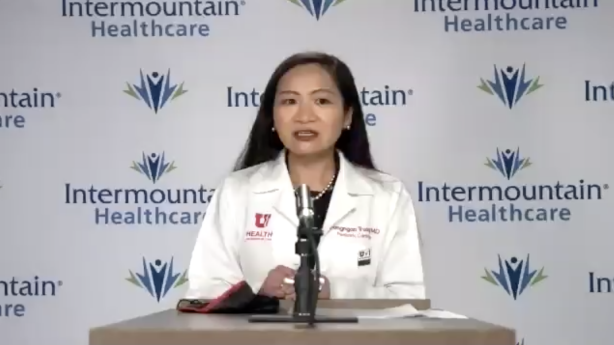
The massive project includes work from more than 30 children’s hospitals in the US and Canada. It is funded by the National Heart, Lung and Blood Institute, said Dr. Ngan Truong, a pediatric cardiologist at the University of Utah Health and Intermountain Primary Children’s Hospital, and the study’s co-leader.
“The MUSIC Study comes at an important time,” she said. “My colleagues and I at Intermountain Primary Children’s Hospital have currently treated dozens of young patients with MIS-C, and we will continue to care for them after their hospitalization.”
The first effects of MIS-C
In October, 12-year-old Madilyn Dayton of Cokeville, Wyoming, woke up in immense pain. She could not move much and ended up in Primary Children’s Hospital, where she was soon diagnosed with MIS-C.
Her family had no idea that she had even been exposed to COVID-19, since no one in the household of eight people had shown symptoms or tested positive for them. What started as flu-like symptoms quickly turned into something much more serious.
Madilyn and her mother, Marilyn Dayton, shared their story late last year. A few months later, Madilyn said that “things are going much better now.”
“I still get tired quickly, but otherwise everything is almost back to normal,” she said, joining her mother in the announcement of the study via video chat.
Marilyn Dayton said she has kept Madilyn out of personal schooling since her diagnosis as a precautionary measure and because of her chronic fatigue. Once an active child who participated in many sports, Madilyn was shot at a basketball after five minutes.
“We noticed the fatigue part,” said Marilyn Dayton. “I don’t know if she can get up and do another whole day of school and take care of everything. She still sleeps a lot. ‘
Much remains unclear about MIS-C, which is why Madilyn will eventually participate in the new long-term study. The complication after the coronavirus leads to all kinds of different reactions, and it is unclear how long they will last.
Truong explained that MIS-C is a rare complication of COVID-19 infection believed to be the result of an “extreme immune response” to SARS-CoV-2. It mainly affects school-age children but has also been reported in infants and young adults. Symptoms include fever, stomach pain, diarrhea, red eyes, rash, and fatigue.
It can lead to serious disease of multiple organ systems, such as the heart, lungs, blood, kidneys, or brain. Children who develop MIS-C are often hospitalized and require intensive care because of low blood pressure, shock, or heart problems.
The total number of children admitted to Primary Children’s Hospital with MiS-C since the start of the pandemic is about 50, but the number is growing, Truong said. The hospital has reported about 30 new cases since mid-November. The increase in MiS-C cases appears to follow similar patterns about an increase in coronavirus-related pediatric hospital admissions in Utah, a study from the University of Minnesota pointed out.
The Centers for Disease Control and Prevention reported 1,626 cases of MIS-C nationwide as of April 2020. It also reported 26 deaths of children who had symptoms that met the definition of the syndrome.
Because the COVID-19 vaccine has not yet been approved for children, experts say the only thing that can slow MIS-C is protective measures to stop the spread of the coronavirus.
Data also shows that a disproportionate number of Black and Latino were affected, Truong added. Still, there aren’t many answers when it comes to understanding the syndrome, such as why some kids end up with it.
“MIS-C has been largely a mystery so far,” she said. “We don’t yet know what risk factors cause some children with COVID-19 infection to develop MIS-C and others not.”
These unknown factors also include whether this can lead to serious long-term effects, such as scarring of the heart, which can lead to serious heart problems and possibly even death. The unknown at the heart is one reason some pediatricians recommend three to six months of recovery before physical activity such as exercise.
Finding answers to long-term effects
Potential long-term effects go beyond the heart. The study could determine how long Madilyn’s documented chronic fatigue will last. It – along with difficulty concentrating – has emerged as a longer side effect of COVID-19 in adults, Truong said.
The researchers will also address the evaluation of long-term effects on the nervous system, lungs, immune system and gastrointestinal system. This will be performed by reviewing hospitalization and follow-up appointment data, as well as annual telephone interviews with participants to monitor their symptoms over time.
Many hospitals already had follow-ups up to six months to check-in MIS-C patients, so the study will look at the results collected from participating hospitals.
“We will also look for genetic clues to disease risks and outcomes,” Truong said. “We will use this information to develop evidence-based treatment guidelines for MIS-C that will help pediatricians better identify and respond to children with MIS-C symptoms.”
I wanted answers … Unless they do such studies and find participants to participate in them, they can’t get those answers.
– Marilyn Dayton
For Truong, she finds the study relevant to the families of children diagnosed with MIS-C. She said she often gets questions from parents who want to know if the symptoms their kids are having at the time will persist in the future – and for how long.
Those are questions she has no answer to.
“Unfortunately, I don’t have a clear answer for them at the moment, and the data we have is very limited at the moment. However, I hope we will have more answers for parents and for my patients in the years to come,” she said. “We hope that the data from the MUSIC study will help us provide guidance and long-term follow-up strategies for children and young adults, for example if we need to limit their activities.”
Marilyn Dayton is one of the parents who asked about her child’s future. Although she and Madilyn wish they had the answers now, they seized the opportunity to participate in the investigation.
It’s something they said they never really had any questions or doubts about.
“I wanted to answer,” said Marilyn Dayton. “Unless they do these kinds of studies and find participants to participate in, they can’t get those answers.”
