
Mutating viruses; so everything really does. But experts are now concerned about some of the thousands of coronavirus variants that have surfaced around the world. We wrote about the British variant last month; now there are more, including one in Los Angeles. You don’t have to panic. But it is good to be informed.
One of the main reasons we are seeing new variants now, one year after the pandemic, is that there are so many more viruses than 12 months ago. The more viruses there are in the world, the more likely it is to mutate. And the more variants there are, the more likely some of them will be bad news.
If we (as a global community) had been better able to contain the virus at all, we might not have gotten to the point where there are multiple variants that are different enough to worry experts. But here we are.
Another thing to remember is that you will only find variants when you search for them. The UK variant, B.1.1.7, was discovered in part because the UK does a lot of so-called surveillance tests – checking exactly what types of coronaviruses there are. The US does some of this too, but much less. The B.1.1.7 variant was probably already in other countries when it was discovered in the UK; they just hadn’t found it yet.
G / O Media can receive a commission
What are the variants you should know about?
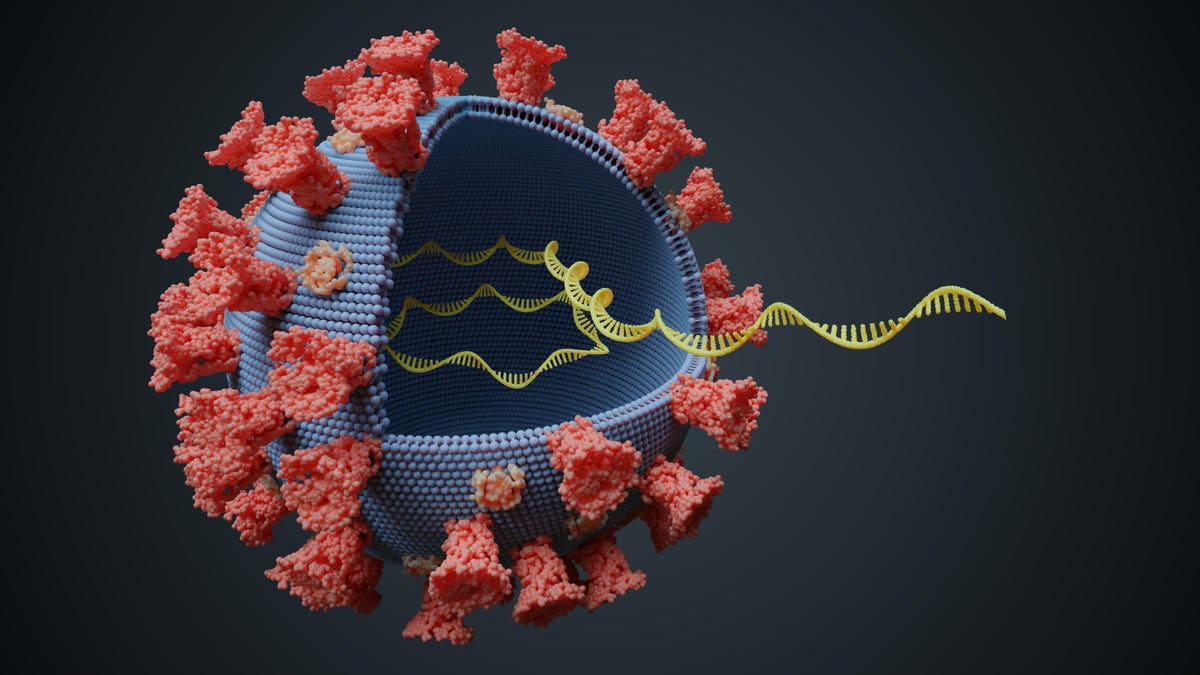
B.1.1.7 was found in the UK in November 2020, where it has probably been circulating since September or earlier. This article in the New York Times has more details about the strain and its mutations. It appears to be 50% more transmissible than a typical COVID virus. It has multiple mutations, including eight on the spike protein.
(The spike protein is the part of the virus that interacts with our cells. When we make antibodies to the spike protein, those antibodies can prevent the virus from infecting us. The mRNA vaccines contain the genetic code of the spike. protein, that allows our cells to make the protein and then make antibodies against it.)
B.1.1.7 is more transmissible, but the disease it causes does not appear to be worse than normal.
B.1.351 was discovered in South Africa, in samples dating back to October 2020, and it also has mutations in the spike protein. It appears to be more transmissible than typical COVID, but does not change the severity of the disease. Both this variant and those from the UK share a mutation called N501Y. A recent study posted as preprint, discovered the Pfizer vaccine is doing seem to protect against variants with this mutation.
P.1 is a variant from Brazil, first discovered in December 2020. It also has mutations that appear to be of concern, including for the spike protein. One of its mutations, E484K, has the potential to evade antibodies; there is some reason to suspect that people who have recovered from a previous case of COVID can be infected by these mutations.
CAL.20C is a variant that is become popular in Los Angeles. We don’t know much about it yet.
Science is still very new for all these variants. The things we know about it are preliminary. None of them seem to cause more serious illness; most are likely susceptible to the existing vaccines; and PCR tests still seem to be able to detect them.
They have also often become the dominant species in their locations, but for some variants, there is a bit of a chicken-and-egg problem determining if they are responsible for spikes in cases or not.
What happens now?
Two things. First, scientists are working to answer the unanswered questions about these variants.
For example, we need to find out whether they are really more transferable, and if so, by how much. We need to know if the variants can evade our natural immunity (which would mean you could catch the virus twice) and if they can evade immunity from the various vaccines and vaccine candidates that already exist. We need to know if one of the variants causes a more serious disease or if there are clinical differences. And we need to strengthen our surveillance in each country to find new variants as they emerge and see where existing variants take over.
If over time it appears that new variants can bypass existing vaccines, the vaccines may need to be updated. We do this every year for the flu vaccine; we may need to do the same for the COVID vaccine.
But the other action point is simpler, albeit still difficult: we all need to do the same things we did for prevention, only to a greater extent. If a variant is more transferable, it is even more important to wear masks and stay at home and take testing seriously. It’s extra, additional important to get vaccines to humans as soon as possible. So in that sense, even if the virus changes, our main measures to combat it haven’t changed.