The UK’s use of genomic sequencing to identify a more contagious strain of SARS-COV-2 has largely served as a wake-up call to inadequate use of the technology in the US.
By mid-December, the US had sequenced about 0.3% of its COVID-19 samples, a rate significantly lower than other developed countries, despite having a quarter of all cases in the world.
In comparison, the UK is in the process of sequencing about 10% of its samples, and Australia is aiming to sequence all relatively limited positive COVID-19 tests there in real time.
“The US has been a no-show for sequencing when you look at the world stage,” said Dr. Eric Topol, Director of the Scripps Research Translational Institute. “Sequencing gives us a lot of different things. It tells us how the virus moves from place to place. It tells us how quickly it changes. We can say it was here on this day, and it was another day. It can tell a super spreader. “
Also see: This is what we know so far about the new species COVID-19
Growing concern about ‘hyper-transmissible’ new strains of SARS-COV-2 has led to increased awareness about the lack of federal funding in the country and the development of the kind of genomic surveillance that has helped the UK to develop the B.1.1.7- strain and South Africa locate the B. 1,351 strain in December.
“We simply don’t have the kind of robust surveillance capabilities we need to detect outbreaks and mutations,” President-elect Joe Biden said Thursday, calling for a dramatic boost in genomic sequencing and surveillance as part of his proposed $ 1.9 Trillion American Rescue Plan.
While a good chunk of federal pandemic dollars so far has been spent on immediate needs such as testing, contact tracking, and helping drug manufacturers scale up their vaccine manufacturing capabilities, experts are now urging the US to push for a stronger genome surveillance system building that can help public health departments identify new tribes while better tackling regional or community outbreaks.
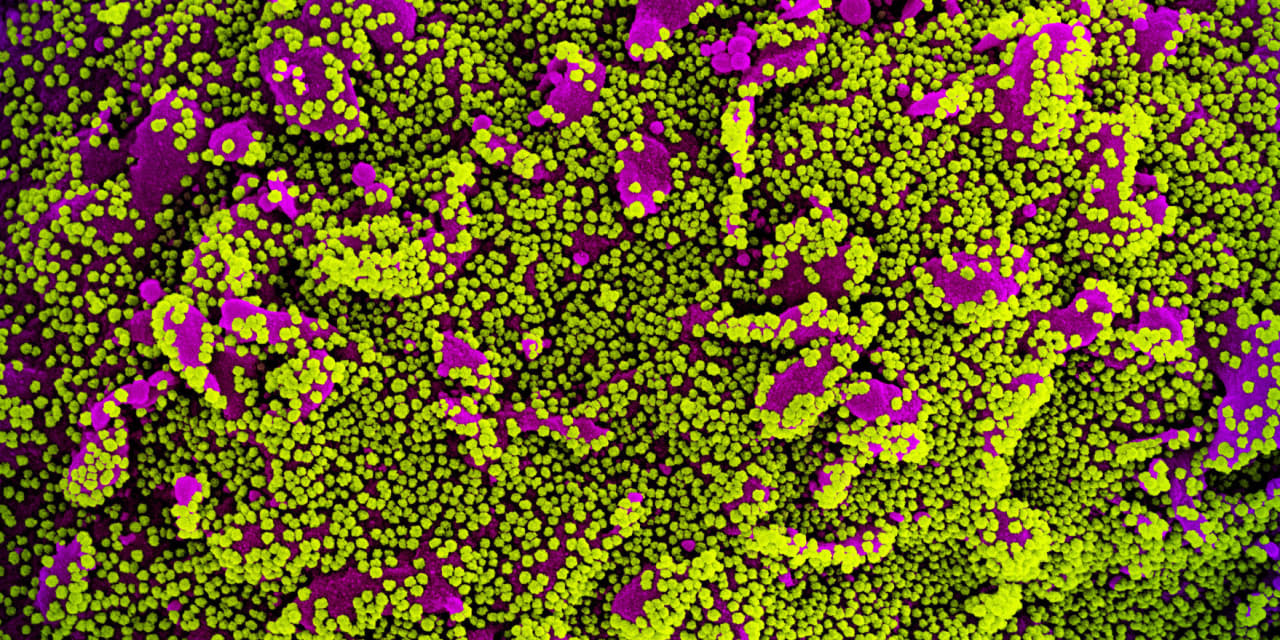
All viruses evolve, and SARS-COV-2 is believed to develop one to two variants per month, although it mutates much more slowly than the flu virus. In mid-2020, researchers began talking about the 614G mutation, which is now considered the dominant form of the virus worldwide. Now concern has shifted to strains B.1.1.7 and B. 1.351, both of which are believed to be more contagious.
According to the Centers for Disease Control and Prevention, as of January 13, the B.1.1.7 strain from the UK has been detected in at least 76 people in 12 states. (The B. 1,351 strain from South Africa has not been identified in the US at this time.)
In the US, where infections, hospitalizations and deaths continue to rise, there has been less emphasis on public health initiatives at the population level when there is so much demand for testing and care.
Read: Biden plans to distribute COVID-19 vaccine doses immediately
Intermountain Healthcare, a Salt Lake City hospital system, sent all positive COVID-19 sequencing tests in the early days of the pandemic. But as cases started to rise and workloads increased, the process began to be disruptive and time consuming, and it was halted, said Dr. Bert Lopansri, Intermountain’s chief of infectious diseases and epidemiology.
“With increasing treatment options, the roll-out of vaccines and the emergence of new variants, upscaling of the sequencing is critical in the future,” he said in an email.
If the US were to sequence at least 5% of positive COVID-19 tests, it would be able to detect emerging strains or variants when they make up less than 1% of the total number of positive cases, according to a model developed by the sequencing company Illumina Inc ILMN,
(Their model will be published this weekend as a preprint, a kind of pre-medical study.)
According to Dr. Phil Febbo, the company’s Chief Medical Officer, this would cost less than $ 500 million by 2021.
Experts say that putting money into a national genomic sequence surveillance network could not only help identify new variants in the future, but help overworked public health departments prioritize who to test, track down and isolate.
It can also be used to inform vaccine manufacturers if there is “an escape strain for vaccines,” a virus strain that could make currently available vaccines less effective or ineffective.
(A study conducted in a laboratory in mice by BioNTech SE BNTX,
and Pfizer Inc. PFE,
showed that their vaccine is still effective against the new strains, according to the Jan. 7 preprint. Moderna Inc. MRNA,
has also said it is confident that the MRNA vaccine will work against the British strain)
“When they see a small cluster of a new variant coming into a community, they can respond quickly,” said Febbo, “and they can make people who are infected aware and do their best to contain that.”
Also see: FDA Identifies 3 COVID-19 Tests Potentially Affected by New Variant
Earlier this month, Illumina announced plans with a private testing company called Helix OpCo to develop a CDC-backed national sequencing monitoring system. Helix is looking for samples of positive COVID-19 assays with the “S gene dropout” for Illumina to sequence. So far they have identified at least 51 cases of B.1.1.7. in the U.S.
Including genomic sequencing in national surveillance isn’t the only way to modernize the way the US can track the virus and take action. In addition to testing, contact tracking and isolation, Topol said this could include genomic sequencing, wastewater monitoring, mobility data collection and the use of digital sensors.
“Now that we get vaccines on full force, we will see the virus contained,” he said. And then there will be places like a whack on a mole where the virus tends to re-emerge. If you’re sequencing, doing wastewater, doing digital, mobility, you basically have a real-time dashboard in the country and you see, ‘Oh, wow, Kalamazoo lights up.’ ”
Illumina shares are up 18% in the past 12 months, while the SPDR S&P Biotech ETF XBI,
won 59% and the S&P 500 SPX,
has won 15%.