Antibiotics have saved countless lives over the decades. But for the pathogens they kill, antibiotics are an old enemy, one they can already fight well.
It turns out that the spread of antibiotic resistance may not be as limited as we thought, giving more species much easier access to antibiotic resistance than previous models lead us to believe.
The findings come from a study conducted by bioinformatics researcher Jan Zrimec of Chalmers University of Technology in Sweden, who looked for signs of mobility between elements of DNA called plasmids.
If a genome were a cookbook, plasmids could be thought of as scraps of paper with prized recipes stolen from friends and family members. Many include instructions for making materials that can help bacteria survive under stressful conditions.
And for bacteria, a dose of antibiotics is about as stressful as it gets.
Although we’ve been using them as medicine for nearly a hundred years, the truth is that we simply took inspiration from a microbial arms race that could be nearly as old as life itself.
As different types of microbes have come up with new ways to stunt the growth of their bacterial competitors over the centuries, bacteria have come up with new ways to overcome them.
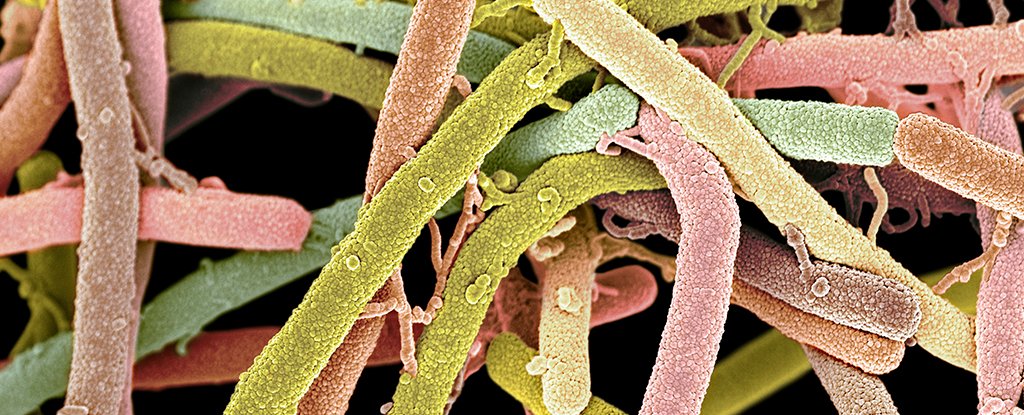
These defenses are often retained in the coding of a plasmid, allowing bacterial cells to easily share resistance through a process called conjugation. If that word brings up thoughts of encounters during prison visits, you have to stretch your imagination a little further to envision it … between unicellular organisms.
To spread plasmids widely between cells in an act of bacterial handkerchief, they must have a region of genetic coding called an origin–from–transfer sequence, or oriT.
This sequence works in tandem with an enzyme that cuts the plasmid so that it can be easily copied and then seals it again. Without oriT, a plasmid’s secret recipe is intended to remain in the owner’s possession.
In the past, it was believed that each plasmid must have both oriT and a code for the enzyme in order to be shared upon conjugation.
Today, it is clear that the enzyme is not necessarily specific for a particular oriT sequence, meaning that if a bacterial cell contains numerous plasmids, some can take advantage of the enzymes encoded by others.
If we want to come up with a catalog of plasmids that can be shared – including those with instructions for antibiotic resistance – we just need to know how much an oriT sequence contains.
Unfortunately, finding and quantifying these sequences is a time-consuming and labor-intensive job. Therefore, Zrimec has developed a much more efficient way to search for oriT based on unique characteristics of the physical properties of the encoding.
He applied his findings to a database of more than 4,600 plasmids and calculated how often mobile plasmids were based on the prevalence of oriT.
As it turns out, we are probably way off in how frequently this essential sequence occurs, with Zrimec’s results being eight times higher than previous estimates.
Considering other transfer factors, this could mean that there are twice as many mobile plasmids among bacteria than we thought, with twice as many bacterial species in their possession. And that’s not all.
There was another discovery that Zrimec made that is concerning.
“Plasmids belong to different mobility groups or MOB groups, so they cannot just transfer a single bacterial species,” Zrimec says.
Yet his research now suggests that half of the oriT sequences he found were suitable for conjugation enzymes from a different MOB group, suggesting that the boundaries between bacterial species may be more permeable to plasmids than we thought.
All of this is troubling news in light of the race to develop new antibacterial treatments.
“These results could imply that there is a robust network for transfer of plasmids between bacteria in humans, animals, plants, soil, aquatic environments and industries, to name a few,” says Zrimec.
“Resistance genes occur naturally in many different bacteria in these ecosystems, and the hypothetical network could mean that genes from all of these environments could be transferred to bacteria that cause disease in humans.”
It’s an arms race in which we’ve made an effort to save lives – we’ve never really imagined how capable bacteria would be to match our firepower.
Such technology will help us better understand what we are dealing with. And although it doesn’t look pretty.
This research is published in Microbiology Open.