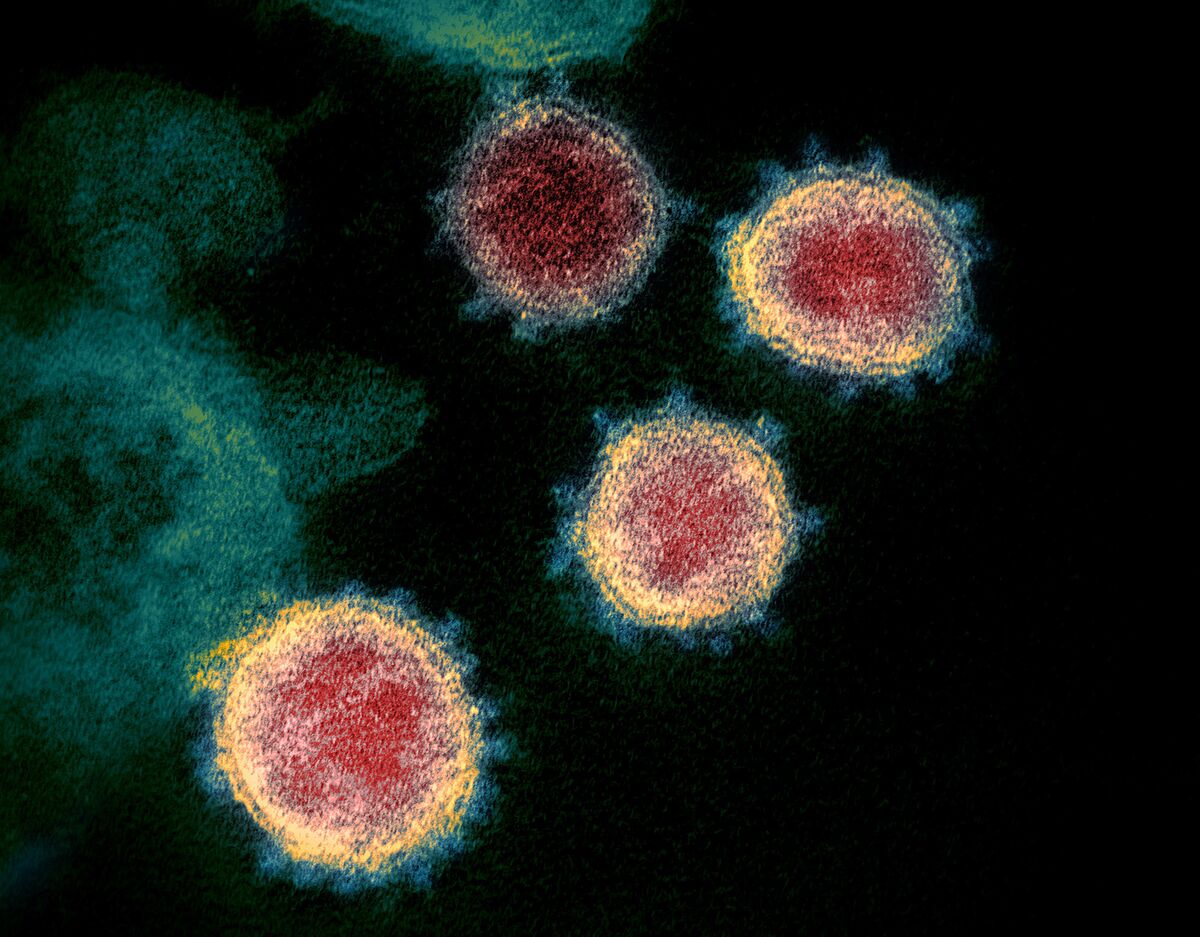

Transmission electron microscope image of SARS-CoV-2, the virus that causes Covid-19.
Source: BSIP / Universal Images Group / Getty Images
Source: BSIP / Universal Images Group / Getty Images
Sign up here for our daily coronavirus newsletter on what you need to know, and subscribe to our Covid-19 podcast for the latest news and analysis.
Then Bette Korber, a biologist joined Los Alamos National Laboratory, saw the first significant mutation in the Covid-19 virus last spring, some scientists were skeptical. They didn’t believe it would make the virus more contagious and said its rapid increase could just be a coincidence.
Now, 11 months later, the D614G mutation she helped discover is ubiquitous worldwide, occur in the genomes of rapidly spreading variants from the UK, South Africa and Brazil. Meanwhile, new mutations are emerging in increasingly complicated patterns, prompting top biologists to devise new ways to track down a fire hose of incoming genomic data.
The goal: to quickly detect variants that could reduce the effectiveness of vaccines for a pathogen that is unlikely to be eradicated anytime soon. The SARS-CoV-2 virus can settle down and become mere annoying like a cold. Or like flu, it could maintain its ability to cause serious illness in some parts of the population, a scenario that could require regular booster shots.

Source: Los Alamos National Lab
“By paying close attention, we can stay ahead of the virus and that’s what everyone is scramble to do now, ”said Korber, who is developing new mathematical tools to detect medically significant variants.
The flow of new genome data is so great that the Los Alamos lab had to upgrade its servers to process the incoming data. Meanwhile, Korber is on four Zoom phone calls a week with experts around the world to come up with criteria for deciding when mutations are worrying enough to merit detailed lab follow-up on how they might affect vaccines.
A major mystery pondered early on by top scientists was what kind of virus the coronavirus will turn out to be. So far, it is more like influenza, which is constantly changing and requires annual revaccination, than measles, a virus so intolerant to mutations that one vaccination regimen can last a lifetime.
“Does this mean we have to make a new vaccine every year?” said Paul Duprex, who owns the University of Pittsburgh Center for Vaccine Research. “We do not know.”
For starters, mRNA vaccines for Covid-19 have an efficacy rate of over 90%, much higher than the 60% rate for flu shots in a good year. But vaccine makers Moderna Inc. and Pfizer Inc., along with its partner BioNTech SE, don’t take any chances. Just in case, they’re already starting booster-shot trials targeting B.1.351, the antibody-evasive strain first spotted in South Africa.
When viruses multiply and copy their genomes, errors can burst the long string of RNA or DNA “letters” that determine how viral proteins are developed. Many of the errors have no effect, or can even make the virus less fit. Only a small percentage of these changes can give the virus a benefit, make it more contagious, or give it the ability to evade the immune system.
The HIV virus is notorious for its rapid mutation rate. In comparison, SARS-CoV-2 mutates much more slowly, in part thanks to a proofreading enzyme that limits changes. But with more than 125 million infections worldwide, some mistakes are bound to break through.
At the same time, the virus has found devious ways to bypass the proofreading mechanism, researchers at the University of Pittsburgh discovered. Rather than making changes to individual RNA letters, groups of multiple letters are deleted at once, apparently undermining the ability of the virus’ natural spell-checking systems to see the change.
74-day race
Some of the first deletions were seen in an immunocompromised cancer patient treated at the University of Pittsburgh Medical Center who died after a 74-day bout with Covid-19. During that time, multiple immune-escape deletions developed, according to Duprex of the University of Pittsburgh, who reported on the cancer patient’s deletions in November.
“Once that damn thing is gone, you can’t fix it,” Duprex said.
What makes the future of SARS-CoV-2 so difficult to predict is that viral evolution is like a three-dimensional game of chess. It is not only the individual mutations that matter, but also the order and combinations in which they occur. A single mutation can alter the virus in subtle ways that alter the impact of others along the line, said Mark Zeller, a scientist at the Scripps Research Institute in San Diego.
Shared mutations
Both the B.1.351 strain that is common in South Africa and the P.1 strain that plagues Brazil share several mutations in the spike protein that the virus uses to access cells. This includes the D614G mutation discovered by Korber, which makes the peak more stable, and the E484K mutation, which is believed to reduce the ability of some antibodies to bind to the peak.
But so far, for reasons not fully understood, it is the B.1.351 that appears to have more impact on Pfizer and Moderna vaccines, at least in lab tests.
Overall, the track record of eliminating viruses is poor, with smallpox being the main example. Despite efforts to eradicate polio, there are still lumps in some countries. According to the current virus, that does not bode well Jesse Bloom, a researcher at the Fred Hutchinson Cancer Research Center that studies viral evolution.
“Vaccination will take the edge off this pandemic in a very substantial way,” said Bloom. “But I don’t think we’re going to eradicate SARS-CoV-2.”
Bloom predicts it will take “several years” for the virus to acquire enough mutations to completely escape existing vaccines. Of the approximately 100,000 possible one-letter mutations for the virus, less than 1% likely will help the virus evade antibodies, he said.
A hopeful scenario
While the virus will continue to evolve in the short term, one of the most hopeful scenarios is that it may no longer be able to take major steps to avoid antibodies that make current vaccines work. In this scenario, there may be a practical limit to how much the virus can mutate and stay fit to invade our cells.
According to Shane Crotty, a researcher at the La Jolla Institute for Immunology, the spike protein must maintain a shape that allows it to efficiently couple with its human receptor.
“There is not an infinite number of possibilities,” he said. It’s like putting your foot in a shoe. It still basically needs to be the right shape and size and it still needs to be recognizable as a shoe. “
Still, evidence from other common cold coronaviruses indicates that they can mutate to bypass the immune system over time.
In a recent study, Bloom and colleagues compared the 1984 version of a cold coronavirus called 229E with a version of the same kind that was circulating in 2016, three decades later. Completely 17% of the RNA letters in a major portion of the spike protein that binds the virus to cells was exchanged as a result of mutations.
To test what this meant for human immunity, they obtained blood samples from 1980s patients who were able to neutralize the 1984 viral strain. These people were likely exposed to the 1984 virus and developing protective antibodies against it.
Faded protections
When the researchers tested the samples against strains of the 229E virus that appeared in the 1990s or later, the protection had faded: only 2 of the 8 blood samples were able to neutralize the 2016 strain, and those two showed a strong reduced activity against the most recent virus.
That gives some hints as to how much could change in the future, if there is enough time. “It’s pretty clear that human coronaviruses are undergoing substantial antigenic evolution,” Bloom said in an interview.
However, it remains unknown whether the virus can maintain its ability to cause serious illness as it mutates and more people gain immunity through infections or vaccines.
In research published in January in the journal Science, disease modelers at Emory University found that a key factor will be whether protection against serious illness lasts significantly longer than protection against mild or asymptomatic reinfections, which is typical of coronaviruses that cause colds.
Although the study was done before the current variants emerged, its basic conclusions hold, said Jennie S. Lavine, a postdoctoral fellow at Emory University.
“What we’re seeing with Covid-19 at the molecular and cellular levels doesn’t conflict with what we’re seeing with endemic coronaviruses,” said Lavine, who was the lead author of the paper. “Immunity is declining, but not everything is declining quickly.”