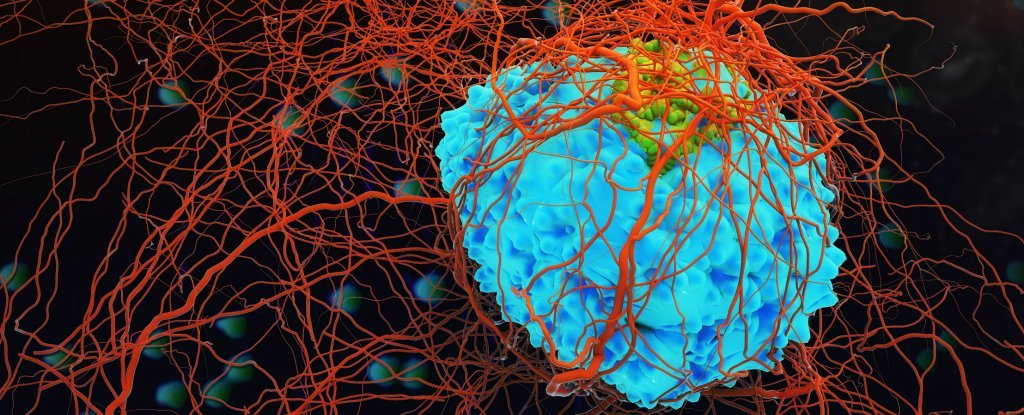
Cancer cells are able to hibernate like ‘bears in winter’ when a threat like chemotherapy attacks them, according to new research – apparently adopting the tactics used by some animals (although they have long been lost in humans) to survive in periods when resources are scarce.
Knowing exactly how to dodge cancers and cope with drug treatments is an important part of working to defeat them for good, and so understanding these hibernation behaviors could play a critical role in future research. Cancers can often recur after remaining inactive or apparently disappearing for several years after treatment.
Preclinical studies on human colorectal cancer cells revealed that they were able to slow down to a low-maintenance, drug-tolerant persister (DTP) state, which would help explain some therapy failures and tumor relapse.
“The tumor acts like a whole organism, capable of dividing itself slowly and conserving energy to help it survive,” said researcher and surgeon Catherine O’Brien of the Princess Margaret Cancer Center in Canada.
“There are examples of animals entering a reversible and slowly dividing state to withstand harsh environments. It appears that cancer cells have cleverly co-opted this state for their survival benefit.”
By collecting human colorectal cancer cells in a petri dish and exposing the cells to chemotherapy, the researchers observed that the colorectal cancer cells go into hibernation in a coordinated manner when chemotherapy drugs were present. The cells stopped expanding, which means that they needed very little nutrients to stay alive.
These observations “also fit into a mathematical model in which all cancer cells, and not a small subpopulation, have an equal potential to become DTPs,” suggesting that these survival strategies can be seen in all cancer cells.
Researchers also used xenografts of colorectal cancer cells on different sets of mice. Once the mice developed tumors of a certain size, the researchers treated the mice with standard chemotherapy regimens. Scientists observed negligible tumor growth in mice treated for eight weeks. When the treatment stopped, tumor growth started again.
Cancer cells removed from the tumors after a regrowth period were then inoculated into different mice and retreated. The regrowed cells remained sensitive to treatments and their growth stopped and started in the same way, findings consistent with cancer cells entering a DTP state.
This DTP state is very similar to a hibernation-like state called embryonic diapause, to which mouse embryos fall back as a sort of emergency survival mode. Embryonic diapause allows many animals, including mice, to effectively pause embryonic development until environmental conditions are more favorable.
Cancer cells have been found here that do a similar trick. Another link between the DTP state and the embryonic diapause is their reliance on a biological mechanism called autophagy, in which cells essentially eat themselves to find the food they need. Autophagy occurs naturally in the body as a way of disposing of waste, but in this case, cancers use it to stay alive.
“We never actually knew that cancer cells hibernated like bears,” says oncologist Aaron Schimmer of the Princess Margaret Cancer Center. “This study also tells us how to attack these sleeping bears so they don’t hibernate and wake up and come back later, unexpectedly.”
“I think this will prove to be a major cause of drug resistance, explaining something we didn’t have a good understanding of before.”
By targeting and inhibiting the autophagy process, the researchers were able to break the hibernation (or DTP) state and kill the cancer cells for good with chemotherapy. This could be an approach to address cancer tumors that are resistant to conventional treatments in the future.
Scientists are already aware of several other ways cancers can hide in the body, so this new study adds to a growing body of evidence on how to target the cancer cells that are most resistant to current drugs and approaches. .
“This gives us a unique therapeutic opportunity,” says O’Brien. “We need to attack cancer cells while they are in this slow-cycling, fragile state before they get the genetic mutations that drive drug resistance.
“It’s a new way to think about chemotherapy resistance and how to overcome it.”
The research is published in Cell.