
We have always had to limit the total number of SARS-CoV-2 infections for reasons beyond the direct risk they pose to those infected. Every new infected person is an opportunity for the virus to evolve in a way that makes it more dangerous – more contagious or more deadly. This is true even if a person has a completely symptom-free infection. The more the virus replicates, the more mutations it will undergo and the more likely something threatening will develop.
One of the disturbing discoveries of the past year was that we don’t have to worry only about the human population. SARS-CoV-2 has been found in a number of species, especially cats and mink, that we spend a lot of time with. From there, it has even spread to the wild mink population, and the virus has jumped back and forth between humans and farmed minks. These animal reservoirs provide additional opportunities for COVID to evolve in ways that make it more dangerous for us – perhaps through mutations that allow it to adapt to the new species.
A group of German researchers have now tested some of the mutations that have appeared in viruses circulating in mink populations, and the news has been mixed. A specific mutation makes the virus slightly less infectious to humans, but reduces the chance that antibodies raised against the virus will recognize it.
A little different
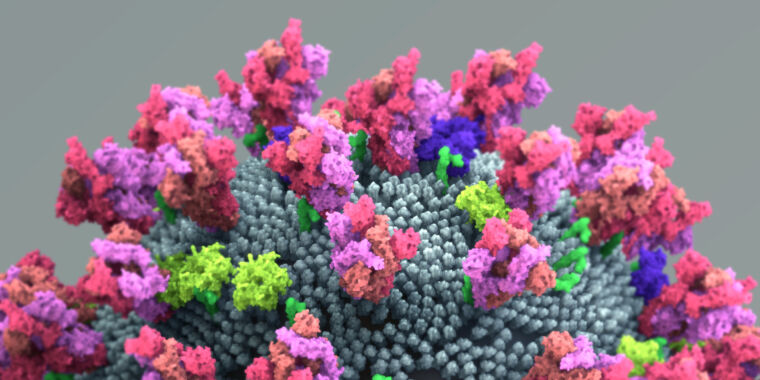
When we first reported on the virus appearing in mink, we only really knew that it picked up mutations while infecting the animals; we were too early to even compile a list of mutations common in mink. That has now changed, and the research team has a list to work with; there is now a catalog of mutations found in European mink farms but not circulating in humans. The researchers focused on mutations in the Spike protein, which the virus uses to attach to and infect human cells. Spike is important because it determines which cells the virus can infect, and it is often the target of antibodies that can prevent the virus from entering the cells.
To look at these mutations, the researchers turned different versions of the Spike protein into a harmless virus and tested whether the manipulated virus could infect cells. They found that certain mutations made it more difficult for Spike to get the virus into some human cells. There were a few more types of human cells it could infect – most notably gut and lung cells, two major sites of SARS-CoV-2 infection. But the virus had a harder time infecting others.
Separately, the researchers looked at how these mutations fared against the antibody response built up after SARS-CoV-2 infection using serum obtained from 14 people previously infected. They focused on a single mutation that is in the part of the Spike protein that clings to the surface of human cells (as opposed to the part that opens the cell membrane).
All but one of the 14 serum samples were able to block infection by the engineered virus without any Spike mutations. But all sera were less effective at blocking infections from viruses carrying a Spike protein altered by a single mutation found in mink. All of them could still block the virus; it just took more serum to do this.
When they examined this more closely, the researchers checked the two antibodies used in a potential COVID-19 therapy from Regeneron. Each of these antibodies by itself is capable of blocking infection of cultured human cells by SARS-CoV-2. But when tested against Spike with the mutation found in mink, only one of the two antibodies still neutralized it. Again, this is consistent with the mutation changing Spike’s profile from the immune system perspective.
What does this mean?
The specific mutation that alters the immune response has also been observed in strains that have adapted to circulate in ferrets, and it is at a site that physically interacts with a human protein. So in all likelihood, this mutation has been selected to allow more efficient infection of mink. In contrast, the mutation has rarely been seen in humans – just one report that it was found in a person with an ongoing infection.
The same virus seems to infect human cells a little less well. This suggests that the current adaptations to mink do not appear to make the virus more dangerous to humans in this regard, although we cannot rule out that further evolution will not have other implications for humans.
Possibly more concerning is the virus’s diminished immune profile. We have developed antibodies that block the virus for use as therapy, and we use them as a measure of an effective immune response. Changes there are thus clearly the attention.
That said, the ability of antibodies to block Spike is reduced, not eliminated. And we are still unsure about the relative importance of neutralizing antibodies to other aspects of the immune response. So while it sounds very bad, it may not have a significant effect on the transmission of the virus to humans. Ultimately, we are likely more at risk for variants evolving in humans, where they are exposed to the actual human immune response.
Still, the study reinforces a more general concern about pandemic management. The virus has spread so widely that it is no longer a matter of taking control of the human population. We must now also be aware of the risk of the virus spreading back to us from any of the domesticated species to which we have transmitted it.
Cell Reports, 2021. DOI: 10.1016 / j.celrep.2021.109017 (about DOIs).