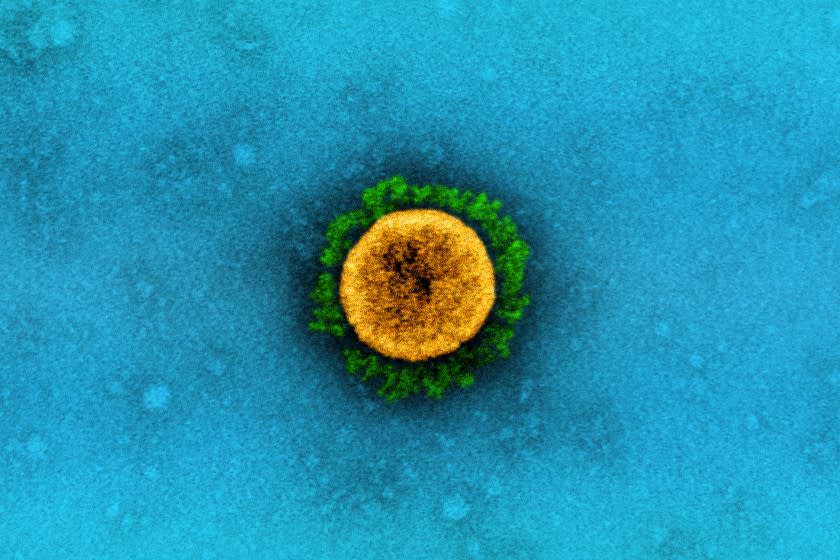
One of the persistent questions of the COVID-19 pandemic is how much immunity people still have after recovering from a coronavirus infection. New research suggests the level of protection is comparable to getting a vaccine – at least for a few months.
Among a group of hundreds of thousands of Americans who tested positive for a SARS-CoV-2 infection, the risk of developing another infection more than three months later was about 90% lower than in people who had not previously been infected and therefore lacked immunity against the virus, said researchers at the National Cancer Institute.
In comparison, when the Pfizer-BioNTech and Moderna vaccines were tested in Phase 3 clinical studies, they reduced the risk of developing COVID-19 by at least 94%.
The findings, published Wednesday in JAMA Internal Medicine, could help formulate plans to return workers to their offices, return students and faculty to school campuses, and reopen a larger share of the economy.
‘I think we knew this, that immunity [after natural infection] takes a long time, ”said Dr. Monica Gandhi, an infectious disease specialist at UC San Francisco who was not involved in the new study. But it is still very exciting. “
There are three important things scientists need to know to understand the biological value of coronavirus antibodies, said Dr. Mitchell H. Katz, who leads NYC Health and Hospitals. They are: do antibodies protect against infection? Can they be reliably detected with current tests? And if they offer any protection, how long will it take?
The new study “provides reassuring answers to the first and second questions,” Katz wrote in a note from the editor accompanying the study.
To investigate immunity from the coronavirus, the cancer researchers examined the results of more than 3 million blood tests administered to Americans between the start of the pandemic and August 23. In total, 378,606 of those tests were positive for SARS-CoV-2 antibodies – a sign that the person providing the sample had an active coronavirus infection.
Among the millions of people tested, some – about 11% of those who tested positive and 9.5% of those who tested negative – later took another test to look for evidence of the coronavirus genetic material in patient samples, which usually collected through the nose, throat or from saliva.
The researchers used these results to see whether people who had a coronavirus infection were less likely than their uninfected counterparts to have SARS-CoV-2 particles in their system. For their analysis, they sorted the results into four groups based on the gap between the antibody test and the genetic test.
After going through the numbers, the researchers found that between 3% and 4% of those who originally tested negative for antibodies to coronavirus later tested positive with the genetic test. This was true for all four time intervals: 0 to 30 days, 31 to 60 days, 61 to 90 days and more than 90 days. The consistency was likely a reflection of the relatively stable rate at which people in their communities were infected at the time, the researchers said.
Compare that with the people who originally tested positive for antibodies against the coronavirus. Their genetic test results were positive at very high rates (11.3%) in the first 30 days, which the researchers say was likely a sign that leftover viral particles were still flushing from their systems.
However, the positivity rate for the genetic test fell to 2.7% in the second month after infection and then dropped to 1.1% in the third month. And after those 90 days, only 0.3% of people with a past coronavirus infection still had an infection that was detected with a genetic test.
That infection rate with the coronavirus was 10 times lower than in people who were probably not previously infected.
That level of protection appears to be comparable to the benefits that the Pfizer and Moderna vaccines provide in their clinical trials, the study authors emphasized.
“Of course, protection provided by a safe vaccine is clearly preferable,” they quickly added, “as the population risk of a severe outcome from an authorized or approved vaccine is expected to be orders of magnitude lower than that of natural ones. infection.”
While the findings may be of great interest to scientists, they are unlikely to make much practical difference at this stage of the pandemic, Gandhi said. That’s because vaccines appear to be at least as protective as past infections, and they’re already being rolled out.
These findings “could have been used two months ago,” she added.
While this study did not gauge how long the benefits of a previous infection last longer than 90 days, other evidence suggests it takes time to wane. For example, Gandhi pointed to an article in Science that found that immune cells activated by SARS-CoV-2 remained in the body for at least eight months.
The findings may help explain why new infections have occurred in Los Angeles County after a devastating holiday spike. Dr. Roger Lewis, director of COVID-19 hospital demand modeling for the LA County Department of Health Services, estimated that about 1 in 3 people in the county now has immunity to the coronavirus.
Still, the study authors said more research would be needed to get a clearer picture of natural immunity to the coronavirus.
“Factors influencing the risk of reinfection – such as varying viral strains, the patient’s immune status, or other patient-level characteristics – should be evaluated in follow-up studies that include more than 90 days follow-up,” they wrote.
This story originally appeared in Los Angeles Times.