Sign up here for our daily coronavirus newsletter on what you need to know, and subscribe to our Covid-19 podcast for the latest news and analysis.
In Mississippi, an online vaccine registry system collapsed in a sudden flow of traffic. Officials at a local health department in Georgia had to resort to counting every dose they received before making appointments. A $ 44 million national vaccine planning and tracking system largely unused by states.
And California, Idaho and North Dakota too few vaccinations because employees forgot to click a “Send” button at the end of the day.
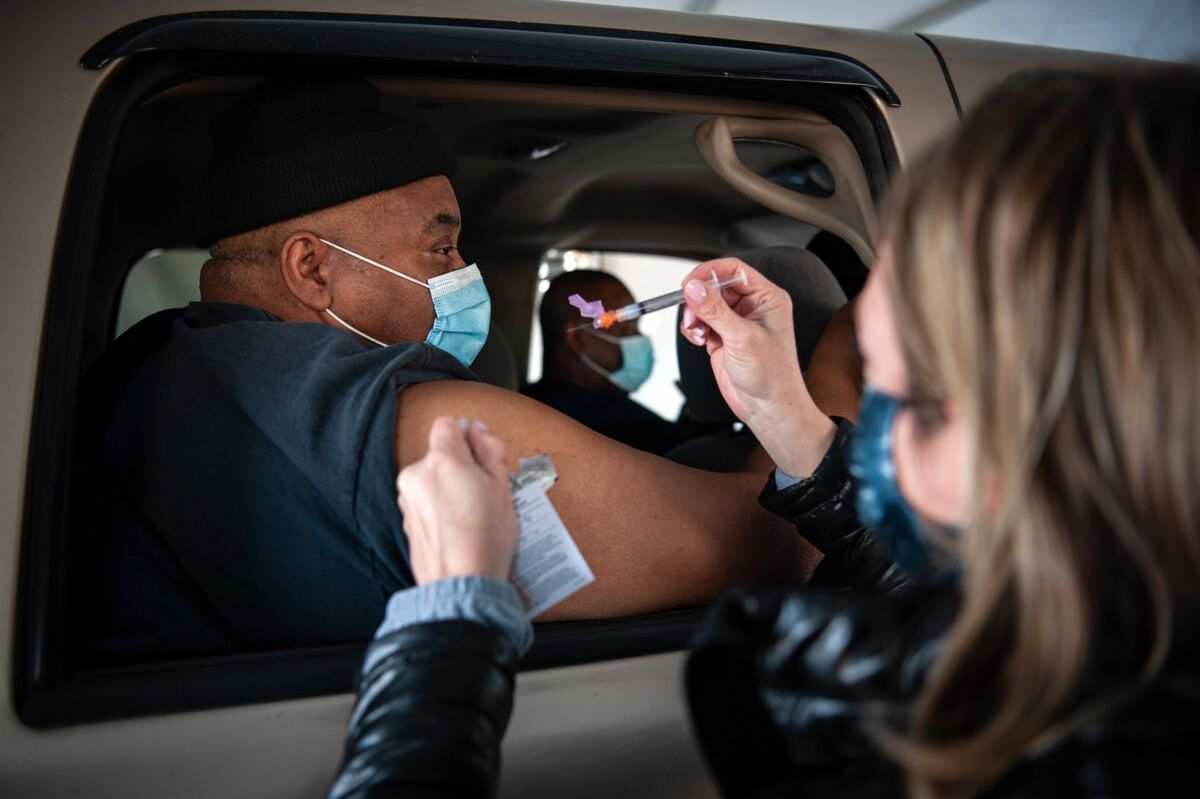
In the US, a vaccination campaign designed to turn the tide of the pandemic and encourage the nation’s economic recovery is stalled by technical glitches and software glitches. Cash-strapped public health departments try to keep their websites from crashing while booking millions of appointments, keeping unpredictable inventory, and tracking how many photos they take.
The situation unfolding in the US, home to technology giants, frustrates an audience eager for the vaccinations. Furthermore, data gaps could distort the national picture of how efficiently vaccines are used if a certain number of doses administered are not counted.
“We feel it is a significant amount,” said Marcus Plescia, chief medical officer at the Association of State and Territorial Health Officials. “That becomes clearer as the data systems improve and we get a better idea of what we are missing.”
Closing gaps
It is a situation that some officials saw coming. Robert Redfield, former director of the Centers for Disease Control and Prevention, cited “years of underinvestment” in public health systems in his testimony to Congress in September. He then said the Trump administration planned to help states plug gaps in IT capacity.
“Hopefully there will be more resources to fill these gaps, as it will be very important that we have reporting for the monitoring and safety of these vaccines,” he said.
Redfield and groups representing state health officials told lawmakers billions in investment would be needed to help states disperse shots. But Congress only allocated that money after it passed a funding bill in late December, after states had already started vaccinating people.
Private companies that provide vaccines face their own problems. Jarred Phillips, his sister, mom and dad each took turns searching the website of Walgreens Boots Alliance Inc. to find a vaccination appointment for his mother. The process involved creating an account, searching by zip code, then by store, by day, and by three-hour time slot.
Nothing came out. Phillips, a 36-year-old technology worker in Wilmington, Delaware, even searched for rural zip codes where there might be light demand. Nothing. Hours later, he couldn’t figure out why the process was so complicated.
“At some point, these solutions have to meet people where they are,” he said.
Walgreens spokeswoman Kelli Teno said the company “has dedicated teams that are actively working on these issues to ensure an easy, safe and transparent experience for all eligible individuals” trying to plan their vaccinations.
Patchwork systems
Like many of the US responses to the coronavirus pandemic, the vaccination effort has been applied in a patchwork. And it’s layered on top of an already fragmented healthcare system. The result is a mishmash of digital systems across the country that has annoyed many of the people trying to use them.
“The biggest mistake was that the government was a little too focused on the first problem: how to get vaccines and ship them to different locations,” said Eren Bali, co-founder and CEO of Carbon Health Technologies Inc. “It was certainly a mistake that didn’t start before.”
About 49 million doses have been distributed across the US so far. About 23.5 million people have received their first of two injections, and 5 million have received both, according to Bloomberg Vaccine Tracker. Last month, Trump administration officials had predicted that 30 million people could be fully vaccinated by the end of January.
Pre-registering people is encouraged to prevent crowds from building up in clinics, especially as the virus is still on the rise in many communities. But sign-ups have been chaotic at times, especially for seniors who are among the first in line for vaccines, with hookup websites that resemble lotteries.
Before appointments are opened, the health departments of Gwinnett, Newton, and Rockdale in Georgia first count inventory. The expected supply can change weekly and the number that actually arrives can differ. The health department relies on Bookly, a web plug-in it started using last year for coronavirus testing.
New appointments open once a week. They are entered in hours.
“It is difficult to communicate with the public when appointments are open,” said Audrey Arona, the director. “I know there is a lot of frustration to be constantly on the website when there are appointments.”
The Georgia Department of Public Health is working on a centralized planning system. The tool is expected to be ready by mid-February, spokeswoman Nancy Nydam said in an email.
In Florida, several counties turned to the ticketing website Eventbrite when the state expanded access to people 65 and older. Los Angeles dropped a software called PrepMod because it couldn’t handle the registration rush. The city turned to Carbon Health instead, which runs a chain of health clinics. The company set up an online tool to find test sites and built a vaccine platform from it.
Follow immunizations
Christ Health staff have spent as much time documenting and reporting vaccinations as they actually administering the shots, said Sam Bagchi, chief clinical officer of the Irving, Texas-based health system. Christ administered about 65,000 doses in Texas, Louisiana, and New Mexico.
The shots are reported in different states depending on who receives them: one electronic patient record for employees, another for the patients and, until recently, paper forms for people who were not patients or staff.
Christ individually manually counts his vaccine inventory and types the data into a web form for the state. Existing systems are not “meant to keep track of what is and what is not given, minute to minute, hour to hour, day to day,” said Bagchi.
Public health technology systems aren’t built for the precision required for the massive vaccination effort, said Joseph Kanter, an official with the Louisiana Department of Health.
“It’s like taking a Yugo and trying to drive 150 on the highway,” said Kanter. “Sometimes the fender falls off.”